How incorporating these foods into our lives to help with optimum nutrition. To radically change the way we live, love and have a sense of vitality EVERY DAY.
Glandular Therapy By Owen Miller, ND
The use of extracts of animal organs containing hormones as well as other substances, some of which have yet to be identified, may be one of the oldest forms of supplement therapy. Although research reviews like Murray and Pizzorno’s Textbook of Natural Medicine offer a favorable perspective, opinion letters like “The Townsend Letter Group” and discussions with other colleagues make glandular therapy appear to be one of the most controversial therapies as well. Anecdotal tributes abound, yet the historical shortage of critical scientific evaluation, arguably in part due to their difficulty or inability as natural substances to be patented and profited from, has in the past caused most of our healthcare community, including some in the “natural” sector, to dismiss the therapeutic value of glandulars altogether. New data may turn some heads, but unfortunately may fail to move those among us who apply the emotionally based “guilt by association” argument that, although apparently meritless, links cow and sheep derived glandulars with concerns like “mad cow” disease. In addition, new data may fail to move those among us who are vegetarians and who impose their personal choice on their patients, following the clear and, I believe, misguided example of our natural health care educational institutions that fail to honor the omnivorous nature of human beings and refuse to allow meat/fish in their student cafeterias or seminar menus and then go on to marginalize glandular therapy in their educational forums. Regardless, I would hope that we all set aside our personal bias and weigh carefully the risk benefit ratio of all of our therapeutic interventions, and in this light consider the historical and current clinically relevant uses of glandular therapy in our patients’ health recovery plans.
Historical Perspective
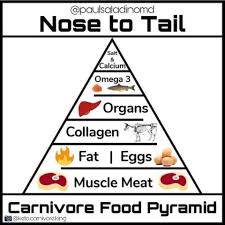
Opinion pieces often date the origin of glandular therapy to the ancient Greeks and Egyptians, apparently following their basic premise that “like heals like”. No, the authors list no references and no, I did not search the “ancient” texts myself. But because people the world over have traditionally eaten every edible part of the animals they “harvest” and only in the last few generations has it become passé to “civilized” Americans and the like (who also happen to be suffering from an epidemic of inflammatory and autoimmune diseases), I decided that the origin of glandular therapy was irrelevant. The point is, glandulars are, and have been for a long time, a valuable part of the world’s diet and the world’s great healthcare systems, including the European model, Ayurvedic medicine, and Traditional Chinese medicine. For more information, check out Protomorphology by Royal Lee (USA) or Live Cell Therapy by Paul Niehans (Switzerland), who both in the first part of the last century championed glandular therapy. Generally the historical motive was to support the weak gland of the patient with an analogous animal gland because they were rich in specific nutrients. Glandular tissues contain replacement hormones and precursor substances that the patient’s body and glands can use to replace, enhance, or rebuild their functions. The hormone angle is pretty clear. American health care providers prescribe thyroid, adrenal, pancreatic and/or gonadal hormones on a regular basis, albeit often of non-bioidentical and synthetic origin. But, to be fair, synthetics have become popular because the hormone content of glandulars has always been tough to quantify. Check the PDR and Drug Facts and Comparisons for natural thyroid to see what I mean (1 grain of desiccated thyroid = 38 mcg levothyroxine (T4) and 9 mcg liothyronine (T3), but it is standardized via iodine content and iodine is only an indirect indicator of hormonal biological
activity). Since our “nutraceutical” supplement manufactures are not able (allowed) to define the relative hormone content it can be frustrating for new doctors to learn how to prescribe these medicines. As a 1985 graduate from Bastyr I was close to clueless, and from my experience working with new doctors it appears that little has changed in this regard. Fortunately, I spent the next year working with Ken Harmon N.D., D.C. and after that Irv Miller N.D., and among the many valuable lessons I learned from these two notable physicians was the value and art of prescribing glandular therapies. It has been a cornerstone of my practice ever since. Personally, I would like to see Bastyr and the other schools of natural medicine take the initiative to pull experienced physicians together on the subject and create a “turn key” prescribing system that they can generally agree upon, and then pass it on to students and practitioners alike. I think the schools are in the best position to lead the charge in evaluating the efficacy and supporting the development of this valuable tool. Hup, hup, hup.
Patient Benefits
Glandular therapy works. Patients on glandular therapy feel better faster. That’s been my experience with a few thousand patients. Sure, diet, rest, and exercise therapies are the primary components of a long term health recovery plan. But the fact is, nobody has that much patience. People come to all doctors wanting results, like yesterday. Since glandular therapy can produce rapid improvements, it enables or encourages patients to continue to apply the difficult diet and lifestyle modifications necessary for their recovery and attainment of higher levels of health awareness and function. We should all be clear that in the beginning it’s not about healing, it’s about preventing harm and relieving symptoms. I consider rapid improvements with glandular therapies to be hormone driven. Stopping the glandular early will most often be met with a decline in patient response and a return of symptoms. I tell patients that real recovery takes time and to continue glandular therapy for at a least a year. I track blood hormone levels along with their symptom picture to determine when and how much to lower or raise their dosages. Recovery although, is determined by variables, like life, that a provider has no control over. Some issues are intractable. Some people are just not willing or able to make the diet and lifestyle changes that would make glandular therapy obsolete, so I keep them on it. It certainly helps and I haven’t seen it hurt at the right dose for a patient in over 20 years, if my memory serves (ok, I’m over 50, so...). Hormone replacement makes people feel better fast. But alone, in the absence of a comprehensive health recovery plan, hormones may only provide a short- term symptomatic benefit while the downside of upregulating target organ function increases the risk of further depletion. I prescribe glandular therapy for a variety of conditions in the context of diet and lifestyle changes, as well as herbal, nutritional, and physical therapies. Classic symptom pictures and lab tests lead the decision making process, but I want to encourage doctors to consider the “vitalistic” perspective of “Body (glandular) Typing”. This evaluation and treatment tool has been around for many decades, but was popularized by Elliot Abravanel M.D. in his 1983 book The Body Type Diet and Lifetime Nutrition Plan. Check it out.
Mechanism of Action
Some portion of the glandular is certainly digested down to source unrecognizable amino acids, fatty acids, etc., but some portion (who knows how much) is absorbed intact and makes its way to the target gland influencing its function. This is why for over 50 years holistic doctors have been prescribing enzymes, like bromelain, papain, and pancreatic enzymes, between meals
to reduce systemic inflammation or to treat cancer. Large molecules are absorbed intact and in sufficient amounts to cause an effect.
In addition to their hormone and nutritional content, glandulars are being recognized by mainstream medicine and used more and more by all types of practitioners for their immune modifying effects. Fifteen to twenty years of laboratory and clinical research are proving the immune benefits with a variety of autoimmune and inflammatory conditions: multiple sclerosis, rheumatoid arthritis, uveitis, diabetes mellitus, graft survival, thyroiditis, myasthenia gravis, asthma, atherosclerosis, colitis, and stroke.
The mechanism of action in this regard is called “oral tolerization” and “bystander suppression”. Basically, when foreign proteins (i.e. collagen) are transplanted or injected into the body the immune system is activated causing a rejection reaction. But when the same foreign particles are ingested, albeit in the presence of intact Peyer’s patches or GALT associated cells (fix digestion first), the immune system is suppressed locally and systemically by several pathways, apparently determined by the amount (dose level) of exposure. High dose single exposure favors clonal anergy/deletion characterized by an absence of T-cell proliferation and decreased interleukin-2 and -2R expression. Repeated low doses (i.e. 0.25 mg of Type II collagen) favor active suppression characterized by an upregulation of T-cells that produce suppressive cytokines, such as transforming growth factor-B1 (TGF-B1) and interleukin-4 and - 10. TGF-B1 suppresses immune function by inhibiting T and B cell division and proliferation.
It also plays a role in tissue repair by attracting macrophages to sites of inflammation and inducing fibrin deposition. These antigen specific regulatory T-cells, generated in the Peyer’s patches and associated cells in response to feeding, migrate to the target organ and suppress ongoing inflammatory reactions, interestingly even if the “antigen” that is consumed and triggers the process is not the antigen in the target organ causing the inflammatory reaction. This is called “bystander suppression”. For example, Type II collagen derived from chicken necks reduces rheumatoid reactions in afflicted joints when ingested even though no chicken collagen started the rheumatoid arthritis in the first place. Direct tolerance is caused when the antigen is consumed and is then later injected or transplanted without causing a reaction.
Safety
Check the literature. I couldn’t find a significant down side to glandular therapy. Granted some commercial ranchers are feeding livestock in a manner that should be considered a “crime against humanity” (i.e. sick cow parts getting into livestock feed) and outlawed internationally. So, it is good to hear from our supplement suppliers about processing technology and the standard of quality that guards our patients from receiving contaminated or weak products. And, yes, we should have a “data bank” to report adverse effects or concerns. Again, I look to the schools to put this together.
Conclusion
In other words there are a lot of good reasons why glandular therapy is good medicine. It is both safe and effective. It provides missing hormones, provides nutrients specific to organ recovery, and suppresses inflammation in the analogous organ. In a social climate of excess consumption and increasing debility and a healthcare context of rampant inflammation and autoimmune activity, the need for glandular therapy is on the rise. Get with the program. Your patients will appreciate it.
Bibliography
Abravanel E. Dr. Abravanel’s Body Type Diet and Lifetime Nutrition Plan. Bantam Books, 2nd edition. 1999.
Alpan O, Rudomen G, Matzinger P. The role of dendritic cells, B cells, and M cells in gut- oriented immune responses. J Immunol. 2001 April 15; 166(8): 4843-52.
Barnett M, Kremer J, St Clair E, Clegg D, Furst D, Weisman M, Fletcher M, Chasan-Taber S, Finger E, Morales A, Le C, Trentham D. Treatment of rheumatoid arthritis with oral type II collagen. Arthritis Rheum. 1998 Feb; 41(2): 290-297.
Bland J. Glandular-based food supplements: helping to separate fact from fiction. Bellevue- Redmond Medical Laboratory, Dept of Chem, University of Puget Sound, Tacoma, WA. 1980: 20-21.
Choy E, Scott D, Kingsley G, Thomas S, Murphy A, Staines N, Panayi G. Control of rheumatoid arthritis by oral tolerance. Arthritis & Rheumatism. 2001 September; 44(9): 1993- 1997.
Collin J. The last word – benefits of usage of animal glandular supplementation. The Townsend Letter Group. 2001.
Faria A, Weiner H. Oral tolerance: therapeutic implications for autoimmune diseases. Clin Dev Immunol. 2006 Jun-Dec; 13(2-4) 143-57.
Friedman A, al-Sabbagh A, Santos L, Fishman-Lobell J, Polanski M, Das M, Khoury S, Weiner H. Oral tolerance: a biologically relevant pathway to generate peripheral tolerance against external and self antigens. Chem Immunol. 1994; 58: 259-90.
Fujihashi K, Dohi T, Rennert P, Yamamoto M, Koga T, Kiyono H. Peyer’s patches are required for oral tolerance to proteins. PNAS. 2001 Mar 13; 98(6): 3310-3315.
Fukaura H, Kent S, Pietrusewicz M, Khoury S, Weiner H, Hafler D. Induction of circulating myelin basic protein and proteolipid protein-specific transforming growth factor-β1-secreting Th3 T cells by oral administration of myelin in multiple sclerosis patients. J Clin. Invest. 1996 July; 98(1): 70-77.
Haas E. Staying Healthy with Nutrition: Complete Guide to Diet and Nutrition. Celestial Arts. 1992.
Maugh T. Fooling the body to heal itself. Los Angeles Times. 1993 October 15.
Millington O, Mowat A, Garside P. Induction of bystander suppression by feeding antigen occurs despite normal clonal expansion of the bystander T cell population. J Immunol. 2004, 173: 6059-6064.
Min S, Hwang S, Park K, Lee J, Lee K, Kim K, Jung Y, Koh H, Do J, Kim H, Kim H. Induction of IL-10-producing CD4+CD25+ T cells in animal model of collagen-induced arthritis by oral administration of type II collagen. Arthritis Research. 2004 March; 6:R213-219.
Murray M. Encyclopedia of Natural Medicine. Prima Publishing, 2nd edition. 1998.
Weiner H, Mackin G, Matsui M, Orav E, Khoury S, Dawson D, Hafler D. Double-blind pilot trial of oral tolerization with myelin antigens in multiple sclerosis. Science. 1993 Feb 26; 259(5099): 1321-1324.
Zhu P, Li X, Wang H, Jia J, Zheng Z, Ding J, Fan C. Oral administration of type-II collagen peptide 250-270 suppresses specific cellular and humoral immune response in collagen-induced arthritis. Clin Immunol. 2007 Jan; 122(1): 75-84.